The Digestive System
790 likes | 808 Views
Discover the different parts of the digestive system and how they work together to break down food. Learn about mechanical and chemical digestion, layers of the GI tract, and the path of food through the body.

The Digestive System
E N D
Presentation Transcript
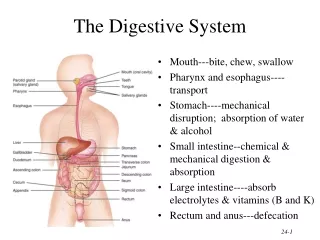
The Digestive System • Mouth---bite, chew, swallow • Pharynx and esophagus----transport • Stomach----mechanical disruption; absorption of water & alcohol • Small intestine--chemical & mechanical digestion & absorption • Large intestine----absorb electrolytes & vitamins (B and K) • Rectum and anus---defecation
Types of Digestion • Mechanical – mouth, stomach,SI, LI • Chemical – mouth, stomach, SI
Layers of the GI Tract 1. Mucosal layer 2. Submucosal layer 3. Muscularis layer 4. Serosa layer
Mucosa • Epithelium • stratified squamous (in mouth, esophagus & anus) = areas of physical stress • simple columnar in the rest = areas for secretion & absorption • secretes enzymes and absorbs nutrients • specialized cells (goblet) secrete mucous onto cell surfaces • enteroendocrine cells---secrete hormones controlling organ function • Lamina propria • loose connective tissue • contains BVs and lymphatic tissue • Muscularis mucosae • thin layer of smooth muscle • causes folds to form in mucosal layer • responsible for local food movements • increases absorption with exposure to “new” nutrients
Submucosa • Loose connective tissue • containing BV, glands and lymphatic tissue • Meissner’s plexus • part of the enteric nervous system - “brain of the gut” • parasympathetic division only - sensory and motor neurons • vasoconstriction of blood vessels to gut • controls contraction of muscularis mucosa • controls the secretory cells of the mucosal epithelium • connected to the myenteric plexus (in the muscularis layer)
Muscularis • areas of skeletal and smooth muscle found • Skeletal muscle = voluntary control • in mouth, pharynx , upper esophagus and anus • control over swallowing and defecation • Smooth muscle = involuntary control • inner circular fibers & outer longitudinal fibers • mixes, crushes & propels food along by peristalsis • Auerbach’s plexus (myenteric plexus) • both parasympathetic & sympathetic innervation of circular and longitudinal smooth muscle layers • part of the Enteric nervous system • controls overall GI tract motility
Serosa • An example of a serous membrane • Covers all organs and walls of cavities not open to the outside of the body • Covering the digestive organs in the peritoneal cavity = visceral peritoneum • Secretes a serous fluid • Consists of connective tissue covered with simple squamous epithelium
Peritoneum • Peritoneum • visceral layer covers organs • parietal layer lines the walls of body cavity • Peritoneal cavity • potential space containing a bit of serous fluid
The path of food: oral cavity/teeth/salivary glands oropharynx/epiglottis esophagus stomach small intestine: duodenum small intestine: jejunum small intestine: ileum large intestine: ascending colon large intestine: transverse colon large intestine: descending colon sigmoid colon rectum anus
Mouth • site of mechanical & chemical digestion • Oral cavity proper • the roof = hard, soft palate and uvula • floor – geniohyoid, mylohyoid – contains the tongue • lips and cheeks-----contains buccinator muscle that keeps food between upper & lower teeth • Vestibule---area between cheeks and teeth
Mouth • Lined with an oral mucosa (stratified squamous epithelium & lamina propria) • Lining of the cheeks = buccal mucosa • Lining of the maxilla and mandible = alveolar mucosa (gingiva) • Landmarks: lingual frenulum, labial frenulum, uvula • Shortened lingual frenulum can impede movement of the tongue within the mouth
Tongue • physiological functions • manipulation of food for chewing and swallowing • production of digestive enzyme • speech • lamina propria layer of the mucosa contains the lingual glands for the secretion of mucus and lingual lipase • extrinsic muscles – control the movement of the tongue in and out of the mouth, manipulates food, hold the tongue in position and forms the floor of the mouth • intrinsicmuscles – originate from and insert into the connective tissue of the tongue, alter the shape and size of the tongue for speech and swallowing
Salivary Glands • Parotid glandbelow your ear and over the masseter • Submandibular glandis under lower edge of mandible • Sublingual glandis deep to the tongue in floor of mouth • All have ducts that empty into the oral cavity (exocrine glands) • Parotid duct open up near maxillary pre-molars • The submandibular and sublingual glands share the same duct – opens on either side of lingual frenulum
Salivary Glands • minor salivary glands • 600 to 1000 glands • small aggregates of secretory tissue present in the submucosa • not found in the gingiva and anterior hard palate • predominantly mucus glands • except the lingual glands (von Ebner’s glands) found on the tongue – open into troughs surrounding the circumvallate papilla • labial, lingual, palatal, buccal, glossopalatine and retromolar glands
Salivary Glands Sublingual gland • Classified either as: serous or mixed • Serous glands - cells secrete a watery fluid – e.g. parotid • Mixed glands secrete both mucus and a serous fluid – e.g. submandibular & sublingual
Saliva • Components: • 1. water • 2. enzymes: amylase, lipase, lyzozyme • 3. mucins, mucus • composition can vary from gland to gland • parotid gland: watery fluid rich in amylase, proline-rich proteins and glycoproteins • submandibular gland also contains higher levels of mucins • 4. multiple electrolytes: sodium, postassium, chloride, calcium, magnesium • 5. glucose, amino acids, urea, uric acid and lipids • 6. secretory Igs – IgG and IgM and IgA • 7. growth factors & hormones: EGF, insulin
Functions of Saliva • 1. buffering – bicarbonate, phosphate ions • protection against demineralization caused by bacterial acids resulting from the breakdown of sugars • 2. Pellicle formation • many salivary proteins bind to the surface of the teeth and oral mucosa – forms a thin film = salivary pellicle • several of these proteins bind calcium to protect the tooth • other pellicle proteins bind bacteria – initial attachment of organisms that produce plaque
Functions of Saliva • 3. maintenance of tooth integrity • saliva is saturated with calcium and phosphate ions • at the tooth surface the high concentration of calcium and phosphate results in maturation of the enamel – increases surface hardness • re-mineralization of lesions upon caries can also be induced by saliva – enhanced by fluoride in the saliva • repair to large areas of enamel breakdown is not possible • 4. antimicrobial action • barrier function provided by mucins • saliva also contains a spectrum of proteins with antimicrobial activity – histatins, lysozyme, lactoferrin and peroxidase • also the presence of antibodies – IgA is the major salivary Ig (results in agglutination of microbes and prevents their adherence to oral tissues)
Functions of Saliva • 5. tissue repair • variety of growth factors are present in saliva • many promote tissue growth and differentiation • 6. digestion • wets food for swallowing – produces the bolus • chemical digestion via amylase and lipase • 7. taste • solubilizes food substances – allows binding to taste receptors located in taste buds
Salivation • controlled by the ANS • parasympathetic system provides a constant supply of saliva to keep the mucus membranes moist and to lubricate the food • Increased salivation – parasympathetic system • sight, smell, sounds, memory of food, tongue stimulation---rock in mouth • stimulation of taste receptors are conveyed to the cerebral cortex to the salivatory nuclei in brainstem- returning impulses via the parasymp system travel via CN 7 & 9 • Decreased salivation – sympathetic system • dry mouth when you are afraid • also inhibits salivation during dehydration
Mumps • Myxovirus that attacks the parotid gland • Symptoms • inflammation and enlargement of the parotid • fever, malaise & sour throat (especially swallowing sour foods) • swelling on one or both sides • Sterility rarely possible in males with testicular involvement (only one side involved) • Vaccine available since 1967
Digestion in the Mouth • Mechanical digestion = mastication or chewing • breaks food into pieces • mixes food with saliva so it forms a bolus • Chemical digestion • salivary amylase • begins starch digestion at pH of 6.5 or 7.0 found in mouth • when bolus & enzyme hit the pH 2.5 gastric juices hydrolysis ceases • lingual lipase • secreted by glands in lamina propria of tongue • begins breakdown of long and medium-chain triglycerides into a free fatty acids and a diglyceride
Digestion in the Mouth • Mechanical digestion = mastication or chewing • breaks food into pieces • mixes food with saliva so it forms a bolus • performed by the teeth • grinding, tearing and shearing of food • two main divisions:crown and root • crown: above gum-line • covered with a layer of enamel • root: secures the tooth in the jaw socket • entry of nerves and blood vessels -innermost layer - pulp (nerves/blood vessels) -outer covering of specialized calcified connective tissue – dentin
Pharynx • Funnel-shaped tube extending from internal nares to the esophagus (posteriorly) and larynx (anteriorly) • Skeletal muscle lined by mucous membrane • Deglutition or swallowing is facilitated by saliva and mucus • starts when bolus is pushed into the oropharynx • sensory nerves send signals to deglutition center in brainstem (medulla oblongata)
Deglutition: Swallowing • Deglutition or swallowing is facilitated by saliva and mucus • starts when bolus is pushed into the oropharynx • sensory nerves send signals to deglutition center in medulla oblongata
Deglutition: Swallowing • 1. Voluntary phase---tongue pushes food to back of oral cavity • stimulates receptors in the oropharynx • message travels to the deglutition center in the MO and lower pons • 2. Pharyngeal stage (involuntary) • breathing stops & air passages are closed • vocal cords close • epiglottis becomes bent over airway (glottis) as larynx is lifted • controlled by autonomic nervous system
Deglutition: Swallowing • 3. Esophageal phase (involuntary) • Peristalsis pushes food down the esophagus • circular fibers behind bolus contract • longitudinal fibers in front of bolus also contract to shorten the distance of travel and widens the esophagus • Travel time is 4-8 seconds for solids and 1 sec for liquids • Lower esophageal sphincter relaxes as food approaches the stomach
Esophagus • Mucosa = stratified squamous • Submucosa = contains large mucous glands • Muscularis = upper 1/3 is skeletal, middle is mixed, lower 1/3 is smooth • upper & lower esophageal sphincters are prominent rings of circular muscle • Collapsed muscular tube • In front of vertebrae • Posterior to trachea • Posterior to the heart • Pierces the diaphragm at the hiatus • Site for hiatal hernia or diaphragmatic hernia
Gastroesophageal Reflex Disease • If lower esophageal sphincter fails to open • distension of esophagus feels like chest pain or heart attack • If lower esophageal sphincter fails to close • stomach acids enter esophagus & cause heartburn (GERD) • for a weak sphincter---don't eat a large meal and lay down in front of TV • smoking and alcohol make the sphincter relax worsening the situation • Control the symptoms by avoiding • coffee, chocolate, tomatoes, fatty foods, onions & mint • take Tagamet HB or Pepcid AC 60 minutes before eating • neutralize existing stomach acids with Tums
Stomach--Chemical Digestion • Protein digestion begins • HCl denatures (unfolds) protein molecules • HCl transforms pepsinogen into pepsin that breaks peptides bonds between certain amino acids • Fat digestion continues • gastric lipase splits the triglycerides in milk fat • most effective at pH 5 to 6 (infant stomach) • HCl kills microbes in food • Mucous cells protect stomach walls from being digested • 1-3mm thick layer of mucous
Anatomy of Stomach • Size when empty • large sausage • stretches due to rugae • Parts of stomach • cardic portion • fundus • body • pyloric portion – narrows at the pyloric sphincter • bolus mixes with gastric juice in the stomach to form chyme • stomach empties as small squirts of chyme leave the stomach through the pyloric sphincter
Muscularis • Three layers of smooth muscle--outer longitudinal, circular & inner oblique • Permits greater churning & mixing of food with gastric juice Serosa • Simple squamous epithelium over a bit of connective tissue • Also known as visceral peritoneum
Mucosa of the Stomach • simple columnar epithelium with embedded mucus cells • forms columns = gastric glands that open into the stomach lumen through gastric pits • gastric glands - for the secretion of gastric juice – mix of water, HCl, enzymes and hormones
Histology of the Stomach - Mucosa • food can remain in the fundus of the stomach for up to one hour before being mixed with gastric juice • during this time – salivary amylase and lipase continue their digestion • after being mixed with gastric juice – these enzymes become inactivated
Cells of the Mucosa • Chief cells: secretepepsinogen (inactive protease)into the stomach which will become pepsin (active protease)– for protein digestion • Parietal cells – secrete: • 1. H+ and Cl- ions into the stomach – become Hydrochloric acid • 2. Intrinsic factor - for the absorption of vitamin B12 for RBC production • Enteroendocrine cells = G cells • secrete gastrin hormone– increases gastric juice production, gastric motility and increase gastric emptying
Parietal Cells • for the secretion of HCl and Intrinsic factor • Intrinsic factor (parietal cells) • absorption of vitamin B12 for RBC production • Hydrochloric acid converts Pepsinogen (from chief cells) into the enzyme pepsin = protein digestion • HCl from the parietal cells is secreted as H+ and Cl- ions • the H+ comes from the absorption of water into the parietal cell – production of HCO3- and H+ ions • proton pumps actively pump H+ into the lumen of the stomach • causes movement of K+ into the parietal cell • the bicarbonate is pumped into the blood in exchange for Cl-ions • opening of K+ and Cl- channels causes the diffusion of these ions back into the lumen
pepsinogen = zymogen (proenzyme) • activation requires the removal of a 44 amino acid peptide • HCl creates an acidic environment • causes the pepsinogen to unfold and cleave itself
Gastric Mucosa Secretions • Parietal cells: HCl and Intrinsic Factor • Chief cells: pepsin and gastric lipase • pepsin – breaks down proteins into smaller peptides • most efficient at breaking the peptide bonds at the N-terminus end of phenylalanine, tyrosine and tryptophan • gastric lipase – like lingual lipase it removes one fatty acid to create a free fatty acid and a diglyceride • lingual and gastric lipases are known as acidic lipases • they do not require bile to function
Absorption of Nutrients by the Stomach • Water especially if it is cold • Electrolytes • Some drugs (especially aspirin) & alcohol • Gastric mucosal cells contain alcohol dehydrogenase that converts some alcohol to acetaldehyde • more of this enzyme found in males than females • 5 different forms of ADH – some more efficient then others
Gastric phase of digestion • starts once food reaches the stomach • stretching of the stomach begins this phase • neural and hormonal regulation to promote gastric secretion and motility
Gastric phase of digestion: Neural Regulation • distension of the stomach stimulates stretch mechanoreceptors – stimulates production of gastric juices • chemoreceptors alsodetect elevated pH (from bolus) – adds to the stimulation • impulses travel via the parasympathetic neurons of the Meissner’s plexus and the Auerbach’s plexus to the cells of the mucosa • stimulates the flow of gastric juice, causes waves of peristalsis to mix the food with the juice and move food into the SI • chemoreceptors monitor pH of the stomach chyme as juice is being made • as the pH of the stomach chyme decreases (becomes more acidic) –creates a negative feedback loop • as the food leaves the stomach and the stretching of the wall lessens – this inhibits this path
Gastric phase of digestion: Hormonal Phase • hormonal regulation: follows the neural phase • distension of the stomach activates the parasympathetic system (red arrows) • parasympathetic system activates the G cells gastrin secretion • secretion of gastrin accelerates the emptying of the stomach via increased muscular contractions (yellow arrows) • gastrin also stimulates the chief cells secretion of pepsinogen
Anatomy of the Small Intestine • 20 feet long----1 inch in diameter • Large surface area for majority of absorption • 3 parts • duodenum---10 inches • jejunum---8 feet • ileum---12 feet • ends at ileocecal valve
Small Intestine • three structures that increase surface area: • plica circularis • permanent ½ inch tall folds in the mucosal layer • not found in lower ileum • cannot stretch out like rugae in stomach • villi • 1 Millimeter tall projections of the mucosa • Core is lamina propria of mucosal layer • Contains vascular capillaries and lacteals (lymphatic capillaries) • absorptive cells with microvilli • cell surface feature known as brush border • The key to the function of the small intestine is its largeSURFACE AREA for absorption
Small intestine mucosa: Intestinal glands Epithelial layer • Absorptive cells– digest and absorb nutrients in the chyme • Goblet cells - Unicellular glands that are part of simple columnar epithelium • Enteroendocrine cells • within the intestinal glands • secretin • cholecystokinin • gastric inhibitory peptide • Paneth cells • secrete lysozyme • kill bacteria
SI mucos: the Lymphatic System • lamina propria of the SI contains areolar connective tissue • plus an abundance of mucosa-associated lymphatic tissue – MALT • solitary lymphatic nodules in the distal part of the ileum • groups of nodes in the ileum – Peyer’s patches
Intestinal glands: Absorptive cells • for the production of brush-border enzymes (“intestinal juice”) • 1 to 2 liters per day • BB enzymes are made and inserted into the microvilli of the absorptive cells • enzymatic digestion by these enzymes occurs externally on these microvilli - rather than in the lumen of the SI • BB enzymes: enzymes for the digestion of carbohydrates, proteins and nucleic acids • as the older cells of the villus are sloughed off and die – burst open and release more enzymes that digest more food in the chyme
Small Intestine: Chemical Digestion -protein and carbohydrate digestion via synthesis of the brush border enzymesby the intestinal glands -enterokinase -maltase, sucrase, lactase, a-dextrinase = smallcarbohydrates and disaccharides -aminopeptidase, dipeptidase = small peptides and dipeptides into amino acids -phosphatases and nucleosidases = nucleotides into nucleosides -resulting monosaccharides, amino acids and nucleotides are internalized by the absorptive cell -SO carbohydrate and protein digestion stops in the interior of the absorptive cell
Small Intestine: Chemical Digestion • BUT - duodenum is also the site for secretion of the pancreatic juice: • 1-2 qt./day------ at pH 7.6 • Pancreas: 5" long by 1" thick • Head close to curve in C-shaped duodenum • pancreatic duct joinscommon bile duct from liver • Opens 4" below pyloric sphincter
Histology of the Pancreas • Acini- dark clusters • 99% of gland • produce pancreatic juice • Islets of Langerhans • 1% of gland – 1 to 2 million • Alpha cells (20%) produce glucagon • Beta cells (70%) produce insulin • Delta cells (5%) produce somatostatin • F cells produce pancreatic polypeptide