“Early Heart Attack Care” EHAC
430 likes | 768 Views
“Early Heart Attack Care” EHAC. Heart Attacks Have Beginnings!. Heart Attack: A Community Problem. With a Community Solution. Course Outline. 1. Anatomy and Physiology 101: Your Heart 2. A Heart Attack in Progress 3. Concepts of Early Heart Attack Care

“Early Heart Attack Care” EHAC
E N D
Presentation Transcript
“Early Heart Attack Care”EHAC Heart Attacks Have Beginnings!
Heart Attack: A Community Problem With a Community Solution
Course Outline 1. Anatomy and Physiology 101: Your Heart 2. A Heart Attack in Progress 3. Concepts of Early Heart Attack Care 4. Recognition and Intervention 5. Delay and Denial 6. You: The Early Heart Attack Care Giver
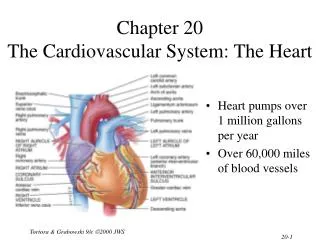
Part 1 Anatomy and Physiology 101: Your Heart
The Human Heart • Location: Middle of the chest • Size: That of a fist • Purpose: Pumps blood throughout the body • Weight: 7 - 12 ounces • Capacity: Pumps 1,800 gallons of blood & beats over 100,000 times daily
The Human Heartand Coronary Arteries SUPERIOR VENA CAVAL BRANCH (NODAL ARTERY) ANTERIOR R. ATRIAL BRANCH OF R. CORONARY ARTERY L. CORONARY ARTERY CIRCUMFLEX BRANCH OF L. CORONARY ARTERY RIGHT CORONARY ARTERY GREAT CARDIAC VEIN ANTERIOR INTERVENTRICULAR (ANTERIOR DESCENDING) BRANCH OF L. CORONARY ARTERY ANTERIOR CARDIAC VEINS SMALL CARDIAC VEIN
The Human Heartand Coronary Arteries SUPERIOR VENA CAVAL BRANCH (NODAL ARTERY) OBLIQUE VEIN OF L. ATRIUM GREAT CARDIAC VEIN SINOATRIAL (S-A) NODE CIRCUMFLEX BRANCH OF L. CORONARY ARTERY SMALL CARDIAC VEIN CORONARY SINUS POSTERIOR VEIN OF L. VENTRICLE R. CORONARY ARTERY MIDDLE CARDIAC VEIN POSTERIOR INTERVENTRICULAR (POSTERIOR DESCENDING) BRANCH OF R. CORONARY ARTERY
Part 2 A Heart Attack in Progress
Heart Attack Facts • #1 Killer of Adults • 4,100 Heart Attacks every day • 600,000 Heart Attack deaths each year • Hundreds of thousands survive but are left with a damaged heart
Three Presentations of aHeart Attack • Sudden, severe pain that stops you in your tracks. • Gradual increasing pain with damage occurring over a period of hours. • Very early presentation with mild symptoms over hours or days.
Ischemia & Angina Pectoris Partial block producing chest pain Area of decreased blood supply
Complete Obstruction: AMI Area of Infarct
Part 3 Concepts of EHAC
Progress: Heart Attack Treatment • Thrombolytic Therapy (clot busters) • Angioplasty • Prehospital Cardiac Care • Decrease in hospital time to treatment saved heart muscle improvement in quality of life
Too Little Progress: Heart Attack Recognition • Only 25% of heart attack victims receive thrombolytic therapy • Only 10% receive therapy within the first critical hour • Most heart attack patients do not benefit from optimal medical advances because of ………………………………….
DELAY • in recognizing and responding to the early warning signs of a heart attack
Why E.H.A.C.? • Early Care: Recognize & Respond • often mild symptoms, usually normal activity • Late Care: Obvious Emergency & Respond • incapacitating pain, diminished activity • Too Late Care: Critical Emergency & Respond • unconscious, CPR, defibrillation, probable death • 85% of the heart damage takes place within the first two hours.
Part 4 Recognition and Intervention
Non-Specific Heart Attack Symptoms: weakness/fatigue clammy/sweating nausea/indigestion dizziness/nervousness shortness of breath neck/back/jaw pain feeling of doom Specific Heart Attack Symptoms: chest discomfort chest pressure chest ache chest burning chest fullness Early Symptoms of a Heart Attack(Prodromal Angina)
Early Signs of Heart Attack(Prodromal Symptoms) • Present in up to half of heart attacks. • Suddenly accelerate preceding the heart attack. • Usually appear within 24 hours before the acute attack but can begin two to three weeks before. • Duration varies from a few minutes to several hours. • Usually intermittent with a pain free period before the onset of acute occlusion.
Part 5 Delay and Denial
Why Do We Delay ? Denial and Procrastination = Our Heart’s Enemy!
1. It’s Nothing Really Serious I’ll just rest a bit
2. I’m Too Busy Right Now I don’t have time to be sick
3. I Don’t Want to be a Problem If it turns out to be nothing I’ll be embarrassed by the fuss made.
4. Paramedics Beware! First responders can easily swayed by patient rationalizations and denials
5. It’s Probably Heartburn or Indigestion I’ll take something for it
6. I’m Strong “Just walk it off, grin and bear it”
7. I’m Healthy I have no serious medical problems I exercise
8. I’ll Just Wait It Out Everything will be OK
Part 6 You: The Early Heart Attack Care Giver
The E.H.A.C. Caregiver • Spouse • Children • Parent • Co-worker • Friend • Exercise partner Anyone who cares about you!
What To Ask and Look For • Do you have any chest discomfort? • Is it tightness, pressure, pain in the center of your chest? • Is the discomfort also in your arms or jaw or neck or throat or back? • Are you sick to your stomach? • Is the person sweaty or clammy? • What were you doing when the symptoms started? • Do the symptoms go away with rest? • Are you having any shortness of breath?
Overcoming Reluctance • Suggest he or she check out early symptoms, better safe than sorry. • Find out the most critical issue on the persons mind. • Call 9-1-1. Paramedics have excellent evaluation tools. • Offer to call spouse or family members if he or she is anxious. • If he or she refuses to seek help, enlist friends or family members to help you convince them. • Be personal and persistent. Sit, talk, try to relieve any tension anddon’t go away. • When he or she agrees, congratulate them on their good judgement. • If all else fails, take charge and be aggressive about getting the patient to the hospital.
A C T W I S E L Y Acknowledge the problem Be Calm Be Tenacious and do not give in. Be Willing to spend the time Be Influential Keep it Simple BeEmpathetic Link the patient with early symptoms to medical care Say Yes - I’ll pay attention A C T W I S E L Y
Listen to your Heart and be a Winner! • Be aware of pressure, not necessarily pain, in your chest. • Be aware if it increases with activity and subsides with rest. • Don’t try to rationalize it away. Be honest with yourself and others. • Call 9-1-1 or have someone drive you to the nearest emergency room. • Don’t go to your doctors office or wait for an appointment. • EHAC is knowing the subtle danger signs and acting on them before damage occurs.
With gratitude for their assistance: Raymond D. Bahr, MD and Jane Strong, RN St. Agnes Hospital, Baltimore, MD Terence D. Valenzuela, MD University of Arizona Captain Richard Hardman, EMT-P Clark County Fire Department, Las Vegas, NV In Memory Of Sally Ann Spackman 1943 - 1998 Designed & developed by: Lani Clark Tucson, Arizona 1998