Understanding the Human Respiratory System: Structure, Function, and Breathing Mechanism
490 likes | 612 Views
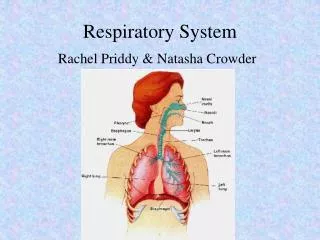
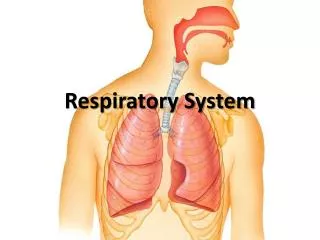
The human respiratory system comprises two main portions: the conductive and respiratory portions. The conductive portion warms, moistens, and filters air, consisting of structures such as the nasopharynx, larynx, trachea, and bronchi. The respiratory portion facilitates gas exchange, removing carbon dioxide and bringing in oxygen via alveoli. The mechanics of breathing involve the diaphragm and rib cage adjusting volume and pressure in the lungs. Understanding these components is crucial for recognizing respiratory health and disease.

Understanding the Human Respiratory System: Structure, Function, and Breathing Mechanism
E N D
Presentation Transcript
Respiratory system Structure, function and disease
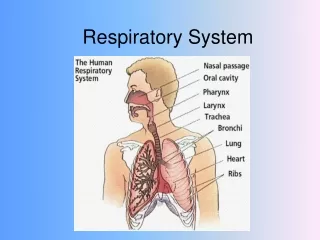
One system, Two Portions, Many Structures.... • Conductive Portion • Warms • Moistens • Filters • Respiratory Portion • Remove waste CO2 • Bring in O2
Branching... • Nasopharynx • Larynx • Trachea • Bronchi • Bronchioles • Terminal bronchioles
Nasopharynx(Upper respiratory passage) • Warming • Bony projections (conchae or turbinates) increase S.A and turbulence (also site for olfactory receptors) • Filtering • Hairs in the vestibules (in the nose!) trap large particles • (Pseudostratified columnar) ciliated epithelia and goblet cells line the interior – known as respiratory epithelium • Cilia beat 250x/minute • about 20 mins to push debris from anterior (front) nostril to the end of the nasopharynx
Lower Respiratory Passages • Larynx • Vocal role • Contain striated muscle and ligaments • Supported by cartilage • Trachea • 10-12cm long, around 2cm in diameter • Lined with respiratory epithelium • 16-20 C-shaped cartilages (hyaline cartilage) support
Still on trachea... • Epithelium + lamina propria = mucosa • Lamina propria contains loose connective tissue • Many elastic fibres • Underneath = submucosa • Connective tissue • Why is the trachea so elastic?
Bronchi (1 = bronchus) • The trachea BIFURCATES to form main bronchi • Structure is very similar to the trachea • Difference: layer of smooth muscle between cartilage and epithelium • Bronchi split into different lobes and different segments of the lungs • Diameter down to around 1mm
A = arteryB = bronchuscart = cartilage platesep = epitheliumSM = smooth muscle of muscularisTM = tunica media of artery
Bronchioles • Thicker smooth muscle than in bronchi (relatively) • No glands or cartilage
Respiratory section • Bronchioles divide into respiratory bronchioles • These form alveoli – most are flattened Type I • 5% are Type II – these secrete a phospholipid to reduce surface tension and prevent collapse • Distance between neighbouring alveoli = 2µm • Walls made up of epithelia and connective tissue with elastic fibres, which contain pulmonary capillaries • Alveoli have no cilia but do have alveolar machrophages • Inside the human body?
Identify the cell types on the next slide. • Look at the proportions of each - can you work out which part of the respiratory system this slide was taken from?
Remember the tissues are 3D – they can be cut through any section and so may appear slightly different
Mechanism of Breathing • Each lung surrounded by a pleural cavity • Diaphragm at the bottom, rib cage around the sides • Breathing in – inspiration - makes the rib cage bigger, increasing the volume and decreasing the pressure relative to the outside • In order to equalise the pressure, air rushes into the lungs
Diaphragm: • Muscular, domed, convex above, squashed in the centre by the heart • Contracts = flattens, increasing the space above it • Relaxes = pushed up by abdominal contents • Ribs: • 12 pairs, top 7 pairs joined to vertebrae behind and sternum in front, next 5 joined to one another and last two are ‘floating’ • 2 sheets of intercostal muscles – internal and external • Contracting intercostals brings the ribs closer together
Regulation • Mostly involuntary but can be overidden • Chemoreceptors • Medulla • Increased CO2, panic reflex • O2 receptors in carotid arteries only kick in when profound hypoxia eg high altitudes
Spirometer • Reflects lung capacity at different points in the ventilation cycle • Consist of a chamber (approximately 6 dm3) suspended freely over water and counterbalanced so that gas passed in or drawn out makes the chamber rise or fall. • A permanent record of the movements of the chamber can be recorded by attaching a pen to it and allowing it to write on a drum revolving slowly (kymograph)
What can it show? • The volume of air that a human breathes into and out of their lungs while at rest is called the tidal volume. This is a relatively small volume of air (around 500 cm3) and provides enough oxygen for a human’s resting needs.
• The maximum amount of air that may be inspired, above tidal inspiration, is called the inspiratory reserve volume. The typical adult value is 2 to 3.2 dm3.• The maximum amount of air that can be breathed out, above tidal expiration is called the expiratory reserve volume. The typical adult value is 0.75 dm3 to 1 dm3.
The vital capacity is the sum of tidal volume, inspiratory reserve volume and expiratory reserve volume. Total lung capacity can be estimated by multiplying the expiratory reserve volume by 6; residual volume can be calculated by subtracting vital capacity from total capacity
Images used in this powerpoint have been taken from: • http://www.courseweb.uottawa.ca/medicine-histology/Default_En.htm • http://www.lab.anhb.uwa.edu.au/mb140/Big/Big.htm • http://www.emptynosesyndrome.org/ • http://www.teachpe.com/anatomy/respiratory_system.php
Lung disease • Fibrosis, asthma and emphysema • All these conditions affect the efficiency of gas exchange at the alveoli
Pulmonary fibrosis • Fibrous tissue grows and divides the lung into separate spaces • This is known as “honeycomb lung” • No-one knows what exactly causes this • It’s possibly a reaction to microscopic lung injuries to which some people are more genetically susceptible • (what might cause “microscopic lung injury”?)
The consequences of PF • The lung epithelium becomes scarred and thickened • So oxygen cannot diffuse efficiently into the blood • The diffusion pathway has lengthened considerably • The volume of air that the lungs can contain is reduced • The lungs lose their elasticity
The symptoms of PF • What do you predict the symptoms to be? • Shortness of breath, especially during exercise • Chronic dry cough – the fibrous tissue obstructs the airway but nothing is expelled • Chest pain – Due to pressure from the fibrous tissue and further damage due to coughing • Weakness and fatigue – Due to reduced oxygen intake
Asthma • The EM shows dust and pollen particles on the ciliated epithelium of the lungs • Asthma is an allergic reaction to these and similar particles • These are called allergens
Asthma Allergens • Dust mite faeces • Pollen • Animal fur • Also asthma triggered/made worse by… • Air pollutants • Exercise • Cold air • Infection • Anxiety and stress
The effect of allergens • White blood cells on the lining of the bronchi and bronchioles release histamine • Histamine has the following effects: • The lining of the airways becomes inflamed • Large amounts of mucus are secreted • Fluid leaves the capillaries and enters the airways • Muscles in the bronchioles contract and constrict the airway
The consequences of histamine release • The above cause resistance to air flow in and out of the lungs • This makes it difficult to maintain a diffusion gradient across the respiratory membranes
Asthma symptoms • What do you think the symptoms may be? • Difficulty breathing • Wheezing when breathing – due to the constriction of the tubes • Tightness in the chest – due to inability to ventilate the lungs properly • Coughing – in response to obstruction
Susceptibility to asthma • The reasons why some people are more susceptible than others are complex and unclear • The incidence of asthma is increasing (USA data shown)
Why the increase? • Asthma tends to run in families (genetic) • Increased air pollution? • Increased stress of modern living? • Increased variety of chemicals in food and manufactured products? • “Cleaner” lifestyles do not expose children to as many antigens and so do not develop resistance?
Emphysema • Emphysema develops in 1 in 5 smokers • It can develop over 20 years • This makes it difficult to diagnose until the lungs are irreversibly damaged
What are the effects? • Healthy lungs are springy • They contain elastic tissue made from the protein elastin • In emphysema, the elastin has become permanently stretched • The lungs cannot force all the air out of the alveoli when we exhale
Alveoli in an emphysematous lung • The surface area of the alveoli becomes reduced • Sometimes they burst • So little or no gaseous exchange takes place
Symptoms of emphysema • Shortness of breath – due to reduced elasticity and reduced surface area • Chronic cough – damaged tissue and mucus are difficult to remove because the ciliated epithelium has been destroyed • Bluish skin colouration – due to low oxygen levels (the next slide contains an upsetting image)
Treatment • None • Lung function cannot be restored and the damage is permanent • However, giving up smoking significantly reduces the rate of further deterioration