MRI
3.38k likes | 4.01k Views
providing mri technique by further knowledge in different organs and systems

MRI
E N D
Presentation Transcript
Outline: MRI technique enable the student to understand different MRI protocols Brain Spine Upper &lower extremity Chest & breast Abdomen &pelvis Special techniques: • MRA • MRCP • MRU • MRSI • FMRI
Objectives: • Explain the MRI scanner types • MRI safety &consideration • Describe the affects of MRI parameters to image quality. • Describe patient preparation for MRI scan procedures. • Describe the type of MRI contrast media. • Describe the patient position &protocols for each part of the body. • At the end of this course the student should be able to understand and explain the following: • Describe the image display &manipulation artifacts.
APPLICATION MRA = Magnetic resonance Angiography , amazed technique which display or show the details of blood vessels ( lumens ), such as circle of wills in brain or any other blood vessel in the body.
ANGIOGRAPHIC TECHNIQUES • Circle of Willis angiograms without any contrast
BRAIN • Indications: • Hemorrhage (stages of) • De myelinating disorders (M.S.) • Infectious processes (encephalitis, meningitis) • Abscesses • Neo plasms • Trauma • Vascular disorders .
BRAIN (cont’d) • Metastasis • Internal auditory canal pathology • Pituitary pathology • Hydrocephalus • Cranial nerve pathology • Congenital anomalies (for anatomical review) • Epilepsy .
SPINE • Radiculopathy • Tumors • Trauma/contusion • Syringomyelia • Metastasis • Vascular disorders • Cord edema • M.S. plaques
SPINE (cont’d) • Caudaequina syndrome • Tethered cord • Arachnoiditis • Marrow-replacing processes • Degenerative disc disease • Discitis • Congenital anomalies
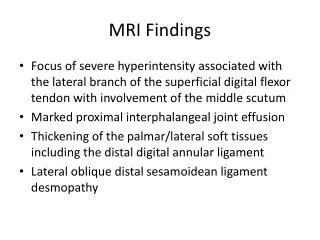
MUSCULOSKELTAL(shoulder, knee, ankle, wrist, elbow, TMJ) • Meniscal pathology • Ligament/tendon injury • Muscle/nerve impingement • Avascular necrosis • Labral tears (shoulder, hip) • Chondromalacia • Inflammation (osteomyelitis) • Primary bone tumours • Soft tissue tumours
ABDOMINAL IMAGING • Breath-hold scans to overcome motion artifact problem • MRCP’s - images of the biliary and pancreatic ductal systems performed non-invasively (no contrast or endoscope!) within seconds • Fetal imaging very diagnostic
ABDOMINAL/PELVIC • Liver pathology • Kidney pathology • Renal artery MRA • Fetal abnormalities
MR Spectroscopy (MRS) • Information obtained is in the form of a spectrum which provides the biochemical information contained within a selected voxel of tissue • Used to detect the absence or presence of a certain compound • Assists in differential diagnosis when standard clinical radiological tests fail or are too invasive
MRS Current Applications • Multiple Sclerosis • Huntington’s • Parkinson’s • Alzheimer’s • Epilepsy • other dementias • metabolic disorders • Stroke • ischemic injury • Tumours and intracranial lesions • Prostate cancer • Encephalopathies
Functional MRI (F MRI) • Detects changes in blood flow or metabolism associated with specific motor or sensory functions or stimuli • Performed by scanning specific areas of the brain/spine while: a) the subject performs a certain motor task or b) exposing the subject to certain external/internal stimuli.
Magnet coil A magnet is a material or object that produces a magnetic field. For details about specific types of magnets see: → Permanent magnet → Resistive magnet → Superconductive magnet An electromagnet whose strong magnetic field (typically at least 0.5 T) is generated using superconductive coils. The conductive wires of the coils are made of a cryogenically cooled Niobium Titanium alloy. Liquid helium is used as the cryogen or liquid nitrogen for pre-cooling. The most important component of the MRI scanner is the magnet.
A permanent magnet is sometimes referred to as a vertical magnet. These magnets are constructed of two magnets (one at each pole).
Permanent Magnet The patient lies on a scanning table between these two plates. Advantages of these systems are: 1) Relatively low cost, 2) No electricity or cryogenic liquids are needed to maintain the magnetic field, 3) Their more open design may help alleviate some patient anxiety. Disadvantages are : 1) Low field strength typically 0.02 T . 2) It has a high weight = HEAVY WEIGHT 3) Poor diagnosis
Resistive Magnet Resistive magnets are constructed from a coil of wire. The more turns to the coil, and the more current in the coil, the higher the magnetic field. These types of magnets are most often designed to produce a horizontal field due to their solenoid design.
Resistive Cont. The main advantages of these types of magnets are: 1) No liquid cryogen, 2) The ability to “turn off” the magnetic field, 3) Relatively small fringe field. The main Disadvantages are : 1) Low magnetic field strength . 2) Always producing heat , and this thing is huge problem for imaging . 3) Not enough for imaging.
Superconducting Superconducting magnets are the most common. They are made from coils of wire (as are resistive magnets) and thus produce a horizontal field. They use liquid helium to keep the magnet wire at 4 degrees Kelvin where there is no resistance. The current flows through the wire without having to be connected to an external power source.
SUPERCONDUCTING MAGNET • No resistance to flow of electricity • Coils of wire surrounded by cryogen bath (Helium) at -273 C • No external source of energy required • Magnetic field present ALL THE TIME!!!
Z Y X Superconducting The main advantages are : The ability of superconducting magnets is to attain field strengths of up to 3 Tesla for clinical imagers, and up to 10 Tesla or more, & good resolution & most common used. Disadvantages are : 1- take more time to produce the image . 2- always making noise with scanning . 3-Not suitable for some care patients. 4- Expensive.
Shim coils Coils that create weak additional magnetic fields in various spatial directions. Used to correct in homogeneity in the main magnetic field.
Gradient coils Coils used to generate magnetic gradient fields. Gradient coils are operated in pairs in the magnet, at the same current, however, of opposite polarities. One of the coils increases the static magnetic field by a certain amount, the opposite coil reduces it by the same amount. This changes the magnetic field overall. The change is the linear gradient. According to the coordinate axes, there are x, y, and z gradient coils.
Gradient coils polarization Gradient coils
RF coils RF coils are the "antenna" of the MRI system that broadcasts the RF signal to the patient and/or receives the return signal. RF coils can be receive-only, in which case the body coil is used as a transmitter; or transmit and receive (transceiver).
T1 WEIGHTING • A short TR and short TE will result in a T1 weighted image • Excellent for demonstrating anatomy • T2 WEIGHTING • A long TR and long TE will result in a T2 weighted image • Excellent for demonstrating pathology
T1 Characteristics • Dark • •CSF • •Increased Water – edema, tumor, infarct, inflammation, infection, hemorrhage (hyper acute or chronic) • •Low proton density, calcification • •Flow Void = less saturation • Bright • Fat • Sub acute hemorrhage • Melanin = melanoma • Protein-rich Fluid • Slowly flowing blood • Gadolinium • Laminar necrosis of an infarct • White matter brighter than Gray
T2 Characteristics • Dark • •Low Proton Density, calcification, fibrous tissue • • Paramagnetic substances – deoxy hemoglobin, methemoglobin (intracellular), iron, hemosiderin, melanin • •Protein-rich fluid • •Flow Void • Bright • •Increased Water – edema, tumor, infarct, inflammation, infection, subdural collection • •Methemoglobin (extracellular) in subacute hemorrhage • Gray matter brighter than white
MRI TECHNIQUE RF pulse sequences , parameters and Artifacts…
RF pulse sequences ,parameters • To create an MR image we need to select a pulse sequence and the scan parameters. The pulse sequence controls the transmission and timing of the RF and gradient pulses which then create a measurable signal from a selected slice. • Every MRI scan begins with an operator-selected scan protocol which may include several different pulse sequences. The operator enters the patient parameters, including identification, location and orientation.
Imaging pulse Sequences • How do we obtain an image with the largest possible contrast between different tissue types? Different tissue types have different transverse magnetizations. Where the signal is strong, the image shows bright pixels; weaker signals result in darker pixels
What determines the signal strength? Clearly to a large degree from the proton density in the respective voxel: the greater the number of protons contributing to the magnetization, the stronger the signal. But even more important for medical diagnostics is the effect of the two relaxation constants T1 and T2 on the image contrast.