MRSA: Beyond Butt Boils
490 likes | 978 Views
MRSA: Beyond Butt Boils. Jeffrey S. Bennett, M.D. Assistant Professor of Pediatrics/Infectious Disease Director, Section of Inpatient Pediatrics University of Kentucky. Educational Goals. History of current MRSA epidemic Describe CA-MRSA, resistance patterns, and virulence factors

MRSA: Beyond Butt Boils
E N D
Presentation Transcript
MRSA:Beyond Butt Boils Jeffrey S. Bennett, M.D. Assistant Professor of Pediatrics/Infectious Disease Director, Section of Inpatient Pediatrics University of Kentucky
Educational Goals • History of current MRSA epidemic • Describe CA-MRSA, resistance patterns, and virulence factors • Antimicrobial Selection • Review invasive and toxin mediated MRSA diseases and their initial treatment • Managing the epidemic – media relations and talking points
Disclosures Dr. Bennett has no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider of commercial services discussed in this CME activity, and does not intend to discuss an unapproved/investigative use of a commercial product/device in this presentation
“Ripped from the Headlines” • Jan 13, 2005 ABC News: 'Superbug' MRSA Worries Doctors, Athletes Drug-Resistant Germ Found in Locker Rooms; Can Kill Within Days • October 17, 2007 Dallas Morning News: U.S. deaths from staph 'superbug' may surpass AIDS deaths • October 19, 2007 Chicago Tribune: Superbug alert at high school; Infection struck 2 football players • October 23, 2007 Wall Street Journal: Putting Superbugs on the Defensive • October 28, 2007 China View News: U.S. county to close all schools amid "superbug" fears (Pike County, Kentucky)
Staphylococcus aureus Basics • Gram’s stain characteristics: spherical, Gram positive cocci in pairs and groups/clusters • Colonize anterior nares, skin of humans and warm-blooded animals (40% of normal population, 50-90% of health care workers); throat colonization increasingly recognized as a potentially important reservoir • Produce a large array of Virulence Factors • Cause a broad spectrum of human disease • Spread most commonly by skin-to-skin contact • Able to survive for extended periods on clothing, surfaces, other fomites
CA-MRSA Basics • CA-MRSA are genetically distinct from hospital-associated strains of MRSA (HA-MRSA) • Major virulence factor 1: antibiotic resistance • mec-A gene: decreased penicillin binding protein affinity (PBP 2a), ß-lactam resistance • erm gene: ribosomal subunit methylation, macrolide/lincosamide/streptogramin resistance • Major virulence factor 2: Panton-Valentine Leukocidin (PVL) • Creates lytic pores in WBC membranes, leads to focal tissue necrosis and rapid abscess (boil) formation
CA-MRSA vs. HA-MRSA*:Same Exterior, but Very Different Under the Hood • Infection Types: CA-MRSA more often associated with skin and soft tissue infection (75%) vs. HA-MRSA (37%) • Age Distribution: CA-MRSA found to be much more common in younger individuals (median age 23 years) vs. HA-MRSA (median age 68 years) • Pulse-Field Gel Electrophoresis Typing: CA-MRSA belong to very different PFGE clonal groups compared to HA-MRSA (genetically different) • Exotoxin Gene Profiles: CA-MRSA commonly carry genes for Panton-Valentine leukocidin (PVL), while HA-MRSA do not • Antibiotic Susceptibility Profiles: CA-MRSA are more likely to be susceptible to a broader range of antibiotics than are HA-MRSA *CA-MRSA: Community-Associated MRSA *HA-MRSA: Healthcare-Associated MRSA Naimi TS, et al. JAMA Dec 10, 2003;290: 2976-2984
Historical Resistance Timeline • 1941: introduction of penicillin • 1944: first reports of penicillin-resistant S. aureus • 1956: discovery of Vancomycin • 1960: introduction of penicillinase-resistant drugs such as Methicillin • 1975: first reports of nosocomialmethicillin-resistant S. aureus (MRSA) • 1983: reports of community-acquired MRSA in children from Ohio, Nebraska, Missouri, Hawaii, New Zealand (majority Clindamycin susceptible)
Resistance Timeline: MRSA • 1996: first report of Vancomycin intermediate resistant S. aureus (VISA) from Japan • 1998 JAMA: 70% of cases of S. aureus disease in a Chicago pediatric hospital are community-acquired MRSA (CA-MRSA, most susc. to clinda, TMP/SMX) • 1999 MMWR: 4 cases of serious, invasive CA-MRSA in children (majority susc. to clindamycin, TMP/SMX.) • 2002 PIDJ: 67% of cases of S. aureus disease in children in Texas Children’s Hospital, Houston, are CA-MRSA • 2010 Infect Control Hosp Epidemiol: 73% of hospital-acquired MRSA at Texas Children’s are CA-MRSA isolates!
Percent of methicillin-resistant Staphylococcus aureus casesclassified as community-associated, 2000–2005* *n = total number of community-associated methicillin-resistant Staphylococcus aureus cases per year Como-Sabetti K, Harriman KH, Buck JM, et al. Public Health Reports. May-June 2009; 124: 427-35
Percent of community-associated methicillin-resistant Staphylococcus aureusisolates by pulsed-field type and inducible clindamycin resistance by year, 2000–2005 ICR 5 inducible clindamycin resistance Como-Sabetti K, Harriman KH, Buck JM, et al. Public Health Reports. May-June 2009; 124: 427-35
MRSA Infections at 25 Children’s Hospitals, 1999-2008 Herigan JC, Hersh AL, Gerber JS, et al. Pediatr 2010; 125:e1294-e1300
S. aureusat University of Kentucky Percent (n=1000) (n=1219) (n=1374) (n=1326) (n=1558) (n=1772) (n=2084) (n=2240) (n=2253) Data from Clinical Microbiology Lab, Chandler Medical Center, University of Kentucky
Interpretation of Microbiology Lab Susceptibility Reports Typical Susceptibility Report for CA-MRSA: • Oxacillin R • Tetracycline S • Gentamicin S • Ciprofloxacin S • Vancomycin S • Trimethoprim- Sulfamethoxazole S • Erythromycin R • Clindamycin S
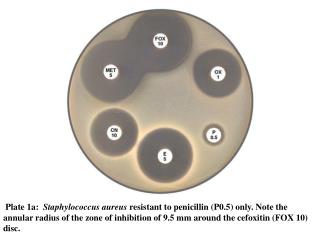
Clindamycin D-Test Erythromycin resistant Clindamycin susceptible (eflux mechanism) Erythromycin resistant Clindamycin inducibly resistant (MLSB)
Antimicrobial susceptibility and inducible clindamycin resistance trends of CA-MRSA isolates, Minnesota Dept of Health, 2000–2005 2000 2001 2002 2003 2004 2005 Chi-square (n=106) (n=145) (n=200) (n=279) (n=434) (n=301) for trend Characteristic Percent Percent Percent Percent Percent Percent (p-value) Erythromycin 45 43 40 28 22 13 92.8 (p<0.01) Ciprofloxacin 80 77 78 68 68 59 26.9 (p<0.01) Clindamycinc 83 83 86 8 86 88 NS Gentamicin 94 97 98 99 99 99 21.9 (p<0.01) Tetracycline 93 94 91 91 94 92 NS Rifampin 97 100 99 99 99 100 NS Trimethoprim- sulfamethoxazole 95 100 99 100 100 99 14.6 (p<0.01) Vancomycin 100 100 100 100 100 100 NS ER-CS 30 35 44 56 64 75 118.4 (p<0.01) ICR 93 82 50 36 16 14 155.9 (p<0.01) Clindamycin total 58 56 64 64 76 77 38.0 (p<0.01) CA-MRSA = community-associated methicillin-resistant Staphylococcus aureus NS = not significant ER-CS = erythromycin resistant/clindamycin susceptible ICR = inducible clindamycin resistance Como-Sabetti K, Harriman KH, Buck JM, et al. Public Health Reports. May-June 2009; 124: 427-35
Antimicrobial Management of Staphylococcus aureusinfections in US Children’s Hospitals, 1999-2008Herigan JC, Hersh AL, Gerber JS, et al. Pediatr2010; 125:e1294-e1300
Is Current Standard Dosing of Vancomycin Adequate? Jimenez-Truque N, et al. Pediatr Infect Dis J 2010;29:368-70. Frymoyer A, et al. Pediatr Infect Dis J 2009;28: 398-402. Standard dose: 40mg/kg/day ÷ q6-8h AUC/MIC >400 associated with optimal outcomes in adults (no pediatric study) CA-MRSAMIC typically <0.5-2 mg/L Current dosing may be inadequate to achieve therapeutic levels in children for MRSA with MIC ≥ 1
Vanc dosing: Lets go to Monte Carlo! Frymoyer A, Hersh AL, Coralic Z, Benet LZ, Guglielmo BJ. Clin Ther. 2010;32:534-42 • A Monte Carlo simulation models known biological variance, replicating real-world conditions over thousands of simulated encounters • i.e. Probability of achieving optimal serum concentrations can be modeled across a range of vancomycin doses against MRSA with different MIC’s • Nifty, huh?!
Evaluating the Empiric Dose of Vancomycin in Pediatric PatientsMcCabe T, Davis GA, Iocono J, Nelson C, Kuhn RJ. (University of Kentucky College of Pharmacy; Pending Submission) Retrospective chart review Jan 08 to Mar 09 Age 1m – 18y Dx: Abscess, Osteomyelitis, and Neutropenic Fever Goal Trough: 15-20 mg/L 239 charts reviewed; 63 patients included in analysis No supratherapeutic levels or renal impairment were noted Calculated: k(hr-1), Vd (L/kg), t½ (hrs) Standard empiric doses of <40mg/kg/day divided q8h 40-60mg/kg/day divided q8h or q6h 60-84mg/kg/day divided q6h Table 4 Proposed Recommendations for Empiric Vancomycin Dosing in Pediatrics* * Assuming normal renal function and fluid status
Time–kill curves of orally available antimicrobials against MRSA. Error bars represent – 1 standard deviation. RIF= rifampicin; SXT=trimethoprim/sulfamethoxazole. Kaka AS, Rueda AM, Shelburne III SA. J Antimicrob Chemother 2006; 58: 680–683
Staphylococcus aureus Virulence Factors • Surface Proteins that promote colonization of host tissues and attachment to host cells: fibronectin • Surface Factors that inhibit engulfment by phagocytes: polysaccharide capsule, protein A (binds IgG, disrupting phagocytosis) • Invasins that promote bacterial spread within tissues: leukocidin (Panton-Valentine Leukocidin/PVL), kinases, hyaluronidase • Biochemical Properties enhancing survival in phagocytes: carotenoids, catalase production • Immunological Disguises: Protein A, coagulase, clotting factor • Membrane-Damaging Toxins that lyse eukaryotic cell membranes: hemolysins, leukotoxin, leukocidin (PVL) • Exotoxins that damage host tissues and provoke disease: Alpha Toxin, Enterotoxins A-G, Toxic Shock Syndrome Toxin (TSST-1), Exfoliative Toxin • Inherent and Acquired Antibiotic Resistance
Panton-Valentine Leukocidin (PVL) A Major CA-MRSA Virulence Factor • PVL-producing CA-MRSA are highly-associated with certain types of infections • Cellulitis • Abscesses • Complicated osteomyelitis • Necrotizing pneumonia and empyema • PVL is not commonly produced by HA-MRSA • May be found in MSSA
Pneumonia • Pneumonia common in S. aureusinfections • 10-20% rate with invasive infection • Many are due to predisposing virus (e.g. influenza) • 2/3 of S. aureuspneumonias demonstrate empyema; necrotizing pneumonia w/o empyema also happens • Pneumonia may be due to septic emboli from other source (osteomyelitis, endocarditis) – nodular pneumonia
PVL-Positive CA-MRSA and Necrotizing Pneumonia • Young, previously healthy patient population • 45% < 1yr • Flu-like prodromal illness; seems benign! • Rapid progression to severe pneumonia and a sepsis syndrome (mortality ~40% within 48 hrs.) • Radiographic appearance: necrotizing pneumonia with cavitary lesions or pneumatoceles, often with pleural effusion, empyema, and/or pneumothorax (pyopneumothorax) • Therapeutic implication: consideration of Clindamycin/Linezolid to inhibit protein (toxin) synthesis, shut off inflammatory cascade
Staphylococcal Pneumonia • Early index of suspicion • Dx by culture of surgical specimen or tracheal aspirate • Vancomycin initial drug of choice • Clinda for uncomplicated cases if local clinda resistance is <10-15% • Vancomycin trough of 15-20mcg/ml suggested • Linezolid shows promise as alternative agent • Early VATS/drainage of empyema may reduce LOS and shorten recovery
Pulmonary Abscess Isolated pulmonary abscess may occur w/o clinical sepsis Primary or secondary Fever, cough, CP, malaise, wt loss May be managed with antibiotics alone if no empyema (Clindamycin)
Endocarditis Fever, malaise, new murmur, splenomegaly, positive blood cultures (usually multiple) Echo aids in diagnosis (Modified Duke Criteria) Embolic phenomena less common in young children (petechiae, Janeway lesions) Septic shock may be evident early or may not develop at all; can by quite indolent (index of suspicion) Typically, vancomycin +/- gentamicin is empiric treatment; vancomycin trough
Osteomyelitis and Septic Arthritis S. aureusis leading cause in all age groups Presents with nonspecific inflammatory symptoms, irritability, and pain Septic hip: surgical emergency Empiric antibiotics often can be safely delayed until aspiration/culture if done within 12 hours MRI is best imaging modality for acute infection
Osteomyelitis: Sites of Involvement Radius 4% Ulna 3% Hands/Feet 13% Humerus 12% Pelvis 9% Tibia 22% Femur 27% Fibula 5%
5% 10% 25% 41% 13% Septic Joint: Sites of Infection 1050 cases of pyogenic arthritis; Principles and Practice of Pediatric Infectious Disease; 2003; p. 475
Osteo and Septic Joint: Managment • Empiric coverage of MRSA appropriate • Preferably after sampling/culture from site • Clindamycin preferred if <10-15% local resistance • Vancomycin trough 15-20mcg/ml is recommended by some experts • Non-operative management of osteomyelitis • No abscess on MRI • Improving clinically with treatment over first week • Repeat imaging, consider surgery if worsening or no improvement
SSSS • Mediated by exfoliative toxins (ETA, ETB) • Fever, widely spread, tender erythema • Quickly form bullae • Nikolsky sign • On path, skin separates at granular layer in the epidermis • Treatment: Supportive care and antibiotic (oral or i.v.) to reduce staph burden
TSS Caused by TSST-1, Staph Enterotoxins B & C (SEB, SEC) Syndrome: Fever, erythroderma, hypotension, and multisystem organ dysfunction (at least 3) Initial GI symptoms, malaise, and dizziness associated with seemingly benign infection or post-op
TSS • TSST-1 inhibits local inflammatory mediator release • Local infection appears surprisingly normal • Identifying source site may be delayed • Eye and mouth: hyperemia, strawberry tongue • Blood culture rarely positive • Organ failure, ARDS in first few days; 3% mortality • DDx: RMSF, Leptospirosis, other bacterial sepsis
TSS: Management • High index of suspicion (phone triage) • Identify and drain/remove source ASAP • 2 peripheral i.v.’s or CVL, intravascular resuscitation • Empiric antibiotics: Vancomycin plus Clindamycin • Intensive care; consider IVIG if not responding to abx • Desquamation 1-2 weeks later is a hallmark of TSS
Severe Sepsis Syndrome • Clinically similar to TSS, but fails to meet criteria • S. aureusisolated from clinical site • Hypotension • ARDS/respiratory failure • at least one other organ system involved • Historically disease of frail, immunocompromised • Increasing in healthy children today; MSSA and MRSA • Mortality rate 60%!! Purpura Fulminans Necrotizing Fasciitis
Management of CA-MRSA Infections • General Rule: choice of empiric therapy should be tempered by the severity of the infection and clinical status of the patient. Infectious Disease specialty consultation may be valuable in guiding diagnosis and treatment. • If a patient with a suspected Staphylococcal infection is being treated a ß-lactam antibiotic (e.g. nafcillin, cefazolin) and is not responding within 24-48 hours of initiation of therapy, the clinician must consider the possibility of MRSA as the etiology.
Management of Active Infection Caused by CA-MRSA • Incise, Drain and Culture whenever possible • Optimal management is based on the severity of illness of the patient you are seeing: • Hospitalization and parenteral antibiotic therapy for: systemic toxicity, bone and joint infections, cellulitis that involves a large area and/or is rapidly spreading, extensive and/or deep-seated cutaneous abscesses not amenable to office drainage, septic shock, necrotizing pneumonia, bacteremia, etc. • Outpatient management and oral antibiotics for: simple, limited-area cellulitis or impetiginous lesions, superficial cutaneous abscesses, etc.
Management of Active Infection Caused by CA-MRSA Empiric antibiotic therapy*: • Outpatient: trimethoprim-sulfamethoxazole (TMP-SMZ), clindamycin, tetracycline (>8 yrs), linezolid (Zyvox) • Inpatient: vancomycin, clindamycin, linezolid, TMP-SMZ, combination therapy (e.g. vancomycin-clindamycin) • The future?: tygecycline (Tygacil), daptomycin (Cubicin), anti-MRSA cephalosporins (Ceftobiprolemedocaril, others in development) *Locate and drain all purulent foci
Conclusions • CA-MRSA infection in children is epidemic and severe infections are now more frequently seen • Accurate interpretation of susceptibility data is an important element in the management of CA-MRSA infection, including empiric dosing • Early identification of CA-MRSA infection, incision and drainage when appropriate, and initiation of appropriate empiric antibiotic therapy are the mainstays of treatment
For More Information CDC Overview of Community-Associated MRSA: http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.html CDC CA-MRSA Fact Sheets for the Public: http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca_public.html CDC Questions and Answers about MRSA in Schools: http://www.cdc.gov/Features/MRSAinSchools/