Understanding Pain Management in Elders: Myths, Facts, and Effective Interventions
520 likes | 629 Views
Effective pain management in elderly patients is crucial yet often misunderstood. Common myths include the belief that pain medications, like opioids, inevitably lead to addiction, while many elders fail to report pain due to fears of dependency or cultural stigmas. Communication among healthcare providers and families is essential for accurate pain assessment and management. This guide explores factual insights, barriers to effective pain relief, non-pharmacological interventions, and the importance of understanding the unique pain experiences of elderly individuals.

Understanding Pain Management in Elders: Myths, Facts, and Effective Interventions
E N D
Presentation Transcript
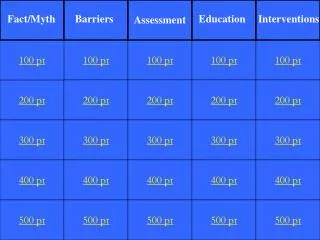
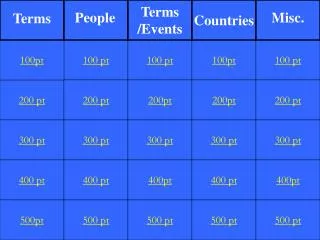
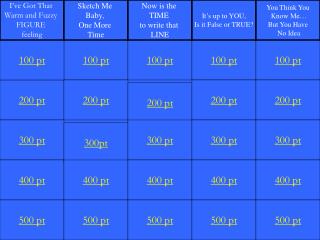
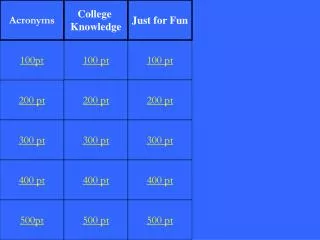
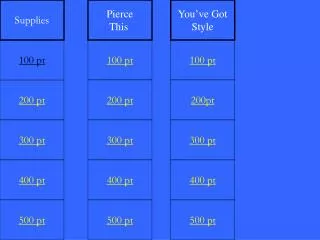
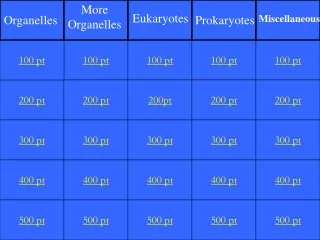
Fact/Myth Barriers Education Interventions Assessment 100 pt 100 pt 100 pt 100 pt 100 pt 200 pt 200 pt 200 pt 200 pt 200 pt 300 pt 300 pt 300 pt 300 pt 300 pt 400 pt 400 pt 400 pt 400 pt 400 pt 500 pt 500 pt 500 pt 500 pt 500 pt
Fact or Myth People who take pain medication (opioids) generally become addicted.
MYTH Less then 1% of those who take opioids for pain become addicted.
Fact or Myth Elders tend to report more pain as they age.
MYTH Many elders tend to not report their pain because they think it is a natural part of growing older.
Fact or Myth Opioids should not be considered when treating elders with severe pain.
MYTH Opioids are the first line of defense we have to combat severe pain. Opioids have no maximum daily dose. This allows us to adjust dose to effective level, no matter how severe.
Fact or Myth Effective pain control improves the ability to fight disease.
FACT One side effect of unrelieved pain is a compromised immune system.
Fact or Myth Constipation is a manageable side effect of opioid use.
FACT A bowel program must always be initiated with opioid use.
True or False Communication is a key component in good pain management.
TRUE Communication must occur between all persons/departments.
Name THREE reasons why families or caregivers may not recognize or believe elders’ reports of pain.
Fear of addiction • Culture • Fear of side effects • Don’t want loved one to be • “targeted or labeled” • Knowledge deficit
Name THREE barriers to good pain management by health care providers.
Personal biases • Inadequate pain assessment • skills • Lack of Knowledge • Lack of Time • Fear of patient addiction
Name THREE barriers to good pain management by Physicians.
Fear of legal issues • Fear of regulatory scrutiny • Unfamiliarity with opioids • Fear of patient addiction • Concern about detrimental • side effects • Lack of communication by • health care personnel and the • patient/family
Give THREE reasons elders may not report pain.
Worry about cost • Fear of addiction • Fear of losing independence • Don’t want to be a bother • Culture • Fear of side effects • Cognitively Impaired • Depression • Low expectations for pain relief
True or False A person’s pain is whatever they say it is and exists whenever they say it does.
TRUE This is the definition advocated by Margo McCaffery & subscribed to by many pain management programs.
Give THREE signs of pain that might be exhibited by cognitively impaired elders.
Changes in emotion (tears) • Changes in movement (restlessness) • Verbal Cues (whimpering, screaming) • Facial cues (grimacing) • Changes in body position (guarding)
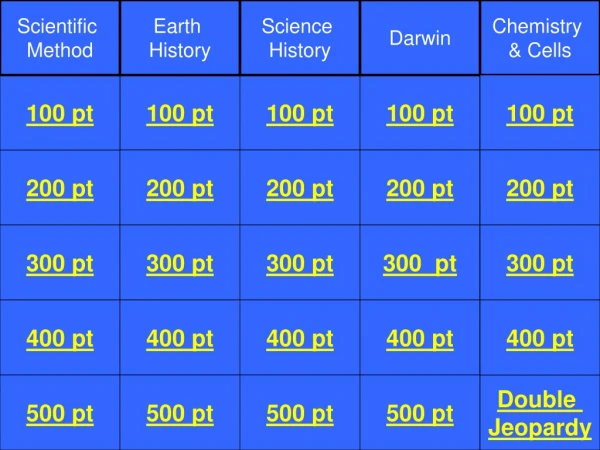
Double Jeopardy What does WILDA stand for? Double Jeopardy
Double Jeopardy Words to describe pain Intensity of the pain Location of the pain Duration of pain Aggravating/Alleviating factors Double Jeopardy
What words might a person use to describe Neuropathic pain?
Shooting • Stabbing • Burning • Tingling • Numbness • Radiating
What words might a person use to describe Somatic and/or Visceral pain?
Somatic – aching, throbbing, gnawing. Viceral – cramping, pressure, deep aching, referred.
True or False Pain medication can not be administered to a person unless they ask for it.
FALSE Staff and family should recognize signs/symptoms of pain in individuals and speak on their behalf.
True or False Nursing is the only discipline that needs to be educated on pain.
FALSE All health care workers are part of the team responsible for providing effective pain management.
Massage Heat/Cold Relaxation/ Imagery Distraction Pastoral Consult Exercise Immobilization TENS Acupuncture Hypnosis
How often should the nurse complete a comprehensive pain assessment?
Admission/Readmission • Change in pain status or health status • Each MDS/OASIS Assessment
Name THREE things to educate the elder and family about when implementing opioids or pain management.
Benefits of effective pain management Options available Goal of treatment Side Effects and their treatment (bowels!) Cost Negative effects of pain Pain symptoms – including nonverbal
True or False The elderly usually have at least three different sites of pain.
TRUE And it is important to assess each pain site separately and document according to WILDA criteria.
List at least three differences between acute and chronic pain.
Acute Short term Sudden onset Usually known cause Usually goes away Typically doesn’t cause severe emotional stress Chronic Often unknown cause/onset Causes depression, sadness, anxiety, anger, loss of control May continue throughout life and requires comprehensive treatment Acute vs Chronic Pain
What are some non-pharmacological interventions that the departments other than nursing can do?
Involve in activities • 1:1 room visits • Aromatherapy • Touch – massage, lotion • Take on walks • Read • Support groups
What can administration do to support effective pain management?
Effective Policies • Adequate Supplies • Training/Education Programs
What does the WHO Ladder stand for and how is it used?