GASTROPARESIS
740 likes | 1.92k Views
GASTROPARESIS. Arnold Wald, M.D., AGA-F University of Wisconsin School of Medicine & Public Health, Madison, WI. MAIN FUNCTIONS OF STOMACH. I . PROXIMAL Functions : Accommodation Storage of ingested food Regulation of intragastric

GASTROPARESIS
E N D
Presentation Transcript
GASTROPARESIS Arnold Wald, M.D., AGA-F University of Wisconsin School of Medicine & Public Health, Madison, WI
MAIN FUNCTIONS OF STOMACH I. PROXIMAL Functions: Accommodation Storage of ingested food Regulation of intragastric pressure Tonic movement of chyme Motor Pattern: Tonic activity • DISTAL Functions: Grinding of food Emptying to duodenum Motor Pattern: Phasic activity
Motility of the Antral Pump Is Initiated by a Dominant Pacemaker in the Mid-corpus Pacemaker potentials determine contractile parameters Fundus Contractile parameters • Max frequency (3/min) • Propagation velocity • Propagation direction Pacemaker region Pacemaker potential Pylorus Antrum Corpus The antral pump is formed by the mid and distal corpus, antrum, and pylorus B3 B87
Onset and Rate of Gastric Emptying Varies With the Composition of the Meal Emptying phase Lag phase 100 Solid meal 75 50 % Meal remaining in stomach Semisolid meal 25 Liquid meal 0 0 20 40 60 80 100 Time after meal (min) B4
Gastric emptying – evolving concepts • Relationship with symptoms unclear • NOT nausea, vomiting or pain • Accelerating gastric emptying does not necessarily improve symptoms • Symptomatic improvement including weight gain is possible without improving gastric emptying Gastroparesis is frequently overdiagnosed on the basis of outdated emptying tests
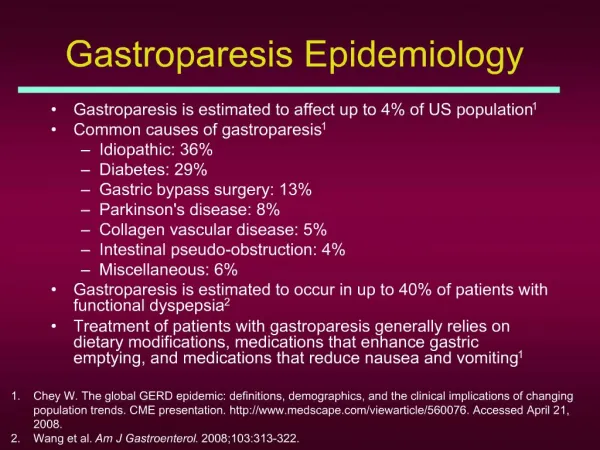
Causes of Gastroparesis • Idiopathic 36% • Diabetic 29% • Upper GI surgery 13% • Parkinson’s 8% • Collagen tissue disorder 5% • Intestinal pseudo-obstruction 4% • Miscellaneous (Incl eating disorders) 6% Soykan et al, DDS 1998; 43:2398-2404
Drugs that delay gastric emptying(Partial listing) β Agonists Anticholinergics Tricyclic agents Phenothiazines Dopamine agonists Opiates Proton pump inhibitors Miscellaneous Dexfenfluramine Antihistamines Lithium Tetrahydrocannabinol Tobacco
Workup for suspectedgastroparesis UGI Series: Excludes mechanical obstruction Retention of barium w/o obstruction is diagnostic Endoscopy: Bezoar without obstruction highly suggestive Gastric Emptying:Solids more sensitive than liquids
Normal values for low fat, egg white GES Lower normal limit Upper normal limit Timefor gastric retention*for gastric retention** 0.5 hr. 70% 1.0 hr. 30% 90% 2.0 hr. 60% 4.0 hr. 10% * Lower value suggests rapid emptying ** Higher values suggest delayed emptying Am J Gastroenterol 2008
2. A 30 y.o. woman with a one year history of type II diabetes mellitus presents with nausea and early satiety. Her blood sugars have been erratic and her last HBAIC was 9.2. Endoscopy was normal and a gastric emptying test showed 20% retention of the meal at 4 hours (normal < 10%). Which of the following would you recommend: • a) Metoclopramide • b) Rigorous control of blood sugars • c) Erythromycin • d) Botulinum toxin injection of the pylorus
Slow gastric emptying was frequent in women with type 2 diabetes with hyperglycemia and normalized after diabetic control J Diabetes & Complications, 2013
2. A 23 y.o. woman developed a viral illness associated with fever, myalgias, nausea, vomiting and diarrhea. Although most of her symptoms resolved over 2 weeks, she continued to have nausea, occasional retentive vomiting, early satiety and a 10 lb. weight loss. Endoscopy showed a modest amount of retained food in the stomach and a gastric retention of a test meal consisting of egg whites, toast and jam at 4 hours was 35% (normal <10%). Which of the following would you recommend first? a) Metoclopramide b) Botulinum toxin injection (pylorus) c) Erythromycin d) Gastric stimulator
Management of Gastroparesis Dietary Modifications Small frequent (6/day) meals Reduced fat (<40 gm/day) Soup, crackers, noodles, pasta, potatoes, rice, cheese Reduced fiber helps avoid bezoar Liquid caloric supplementation
Prokinetic Agents • ACh-esterase inhibitors: pyridostigmine • Motilides:erythromycin • Antidopamine agents:domperidone* • Antidopamine/serotonin agents: • metoclopramide • Serotonin agents:tegaserod*, prucalopride* *Not available in USA
ERYTHROMYCIN • Motilin agonist • No antiemetic effect • Stimulates antral contractions (IV >> PO) • Stimulates MMC • Dose: 125-250 mg bid/tid (PO) 3 mg/kg q 8 hours (IV)
Metoclopramide • Central/peripheral D2 antagonist and 5 HT agonist • Increases antral contractions • Decreases fundal relaxation • Improves antroduodenal coordination • Dose: 5-20 mg qid (PO, IV, SQ, SL)
Metoclopramide • 30% of patients experience side effects • 10% have neurologic side effects Parkinson-type syndrome Tardive dyskinesia • Hyperprolactinemia * Boxed Warning for chronic use issued by FDA*
Domperidone • Peripheral D2 antagonist • Increases antral contractions • Decreases fundal relaxation • Improves antroduodenal coordination • Dose: 10-30 mg qid (PO) Limited availability in USA
Efficacy of Domperidone in Diabetic Gastroparesis □Improved symptoms in 64% □ Improved gastric emptying in 60% □ Reduced hospital admission in 67% □ 28 trials (19 double arm); 1016 patients Sugumar A et al, CGH 2008
Effects of Botulinum Toxin on GE and GI Symptoms Friedenberg FK, et al. Am J Gastro 2008
3. A 28 y.o. man with IDDM is referred for chronic and recurrent nausea and vomiting. He reports 3-4 episodes yearly for the past 5 years with frequent ED visits or hospitalizations lasting 3-4 days. Between episodes, he feels well and has lost no weight. During these episodes, he finds great relief when taking hot showers. The most appropriate intervention for this patient is: • a) Domperidone 20 mg AC meals • b) Nortriptyline in doses up to 100mg hs • c) Discontinue smoking marijuana • d) Strict control of blood sugars; metoclopramide 10 mg SQ during episodes
Cyclic Vomiting Syndrome Recurrent and stereotypical episodes of severe nausea and vomiting separated by symptom free intervals - Gastric emptying rapid or normal - Maintenance of weight
Cannabinoid Hyperemesis - Cyclic vomiting syndrome - Compulsive hot water bathing - Poor response to TCAs
Cyclic Vomiting in Adults(Non-Cannabinoid) • Association with migraine headaches • Psychological disorders (anxiety/depression) • Absence of compulsive hot water bathing • Often responds to TCAs
References 1. Hasler WL. Gastroparesis: pathogenesis, diagnosis and management. Nat Rev Gastroenterol Hepatol 2011;8:438-53. 2. Choung RS et al. Cyclic vomiting syndrome and functional vomiting in adults. Neurogastroenterol Motil 2011;24:20-26