MALABSORPTION
550 likes | 749 Views
MALABSORPTION. פרופ' יוסף צימרמן גסטרואנטרולוגיה המרכז הרפואי של הדסה והאוניברסיטה העברית, עין כרם, ירושלים. MALABSORPTION. GENERALIZED : Non specific impairment in the absorption of multiple nutrients; Pancreatic insufficiency Short Bowel Syndrome

MALABSORPTION
E N D
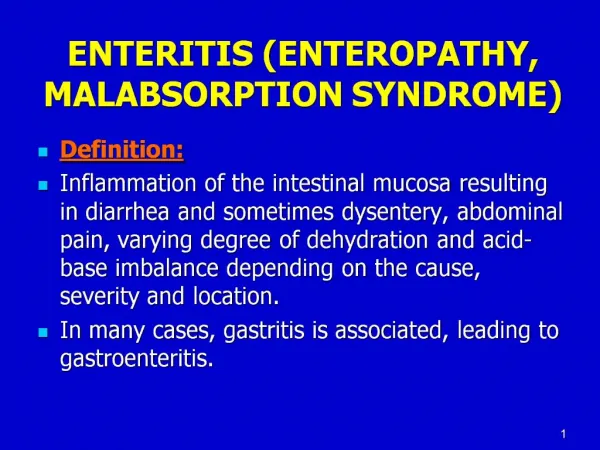
Presentation Transcript
MALABSORPTION פרופ' יוסף צימרמן גסטרואנטרולוגיה המרכז הרפואי של הדסה והאוניברסיטה העברית, עין כרם, ירושלים
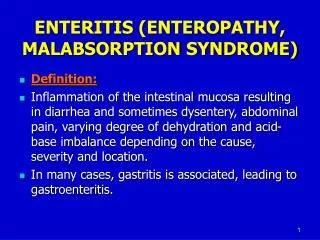
MALABSORPTION • GENERALIZED: Non specific impairment in the absorption of multiple nutrients; • Pancreatic insufficiency • Short Bowel Syndrome • SPECIFIC: Impairment of digestion or absorption of a single nutrient; • Lactase deficiency
When Should We Suspect Malabsorption? • Nutritional deficiencies (anemia, osteoporosis), mainly if dietary intake appears appropriate; • Weight loss; • diarrhea;
Malabsorption: Physical Signs • Non specific: wasting, bloated abdomen, edema and signs of specific nutrient deficiency (glossitis, angular cheilosis, petechiae, etc.) • May suggest a diagnosis (clubbing in small bowel disease etc.)
Pathophysiology • LUMINAL FACTORS (MALDIGESTION) • MUCOSAL FACTORS • Impaired hydrolysis (dissacharidases, peptidases) • impaired transport; • POST MUCOSAL FACTORS • Vascular • Lymphatic
TG DIGESTION:GASTRIC PHASE • Initial hydrolysis by the lingual and gastric lipases. • These lipases, unlike the pancreatic lipase, are active at an acid pH (4.5-5.4) and hydrolyze TG to diglyceride and free fatty acid (FFA). • While their contribution to overall fat digestion in the normal adult is small, they are important in neonates and in patients with cystic fibrosis.
LIPID EMULSIFICATION IN THE STOMACH • Dietary fat, which is partly hydrolyzed by gastric and lingual lipases, is dispersed in the gastric contents in small droplets, creating a lipid emulsion. The motor activity of the antrum is essential in this process. • The emulsion is stabilized by FFA’s released from dietary TG through the action of the lingual and gastric lipases in the stomach .
GASTRIC EMPYING • Delivery of chyme from the stomach is delicately adjusted so it enters the duodenum at a controlled rate, allowing mixing with pancreatic secretions and bile. • Control of gastric emptying is thus critical to ensure optimal digestion.
Stages of Fat Digestion and Absorption:Intestinal Phase • Hydrolysis (pancreatic lipase); • Solubilization in bile salt micelles; • Transport across the luminal membrane of the enterocyte; • Resynthesis of TG in the enterocyte; • Incorporation of TG into chylomicrons; • Elimination of the chylomicrons by the lymphatic system
Properties of the Pancreatic Lipase • Secreted in active form (not proenzyme); • Interfacial enzyme, positional specificity; • Secreted in great excess; • Optimum activity at pH ~6; • Destroyed by acid (pH<3); • Requires co-lipase;
Bile Salt Micelle formation • In order to solubilize fat, bile salts must form micelles; • The formation of micelles depends on the concentration of bile salts, and occurs when their concentration is > 1.5 mmol/L (CMC). • Normally, the bile salt concentration in the duodenum during meal is 5-10 mmol/L.
FUNCTIONS OF INTRALUMINAL BILE SALTS • Micellarsolubilization of fat-soluble vitamins (A,D,E,K)-essential for their absorption; • Micellarsolubilizationof fatty acids and monoglycerides; • Protection of pancreatic lipase against tryptic digestion.
Normally, fat absorption is completed in the upper 2/3 of the jejunum. • Fat malabsorption may result from the following: • Defective mixing; • Reduced solubilization; • Decreased lipolysis; • Decreased mucosal absorption and chylomicron formation; • Defective lymphatic transport of chylomicrons;
CONSEQUENCES OF FAT MALABSORPTION • Steatorrhea; • Weight loss; • Diarrhea; • Deficiency in fat-soluble vitamins;
Sudan Stain Test : A Qualitative Fecal Test for Steatorrhea
FAT BALANCE: THE TEST FOR STEATORRHEA • Chemical determination of fecal fat excretion on a defined fat intake (70-100g/day). • Requires a complete collection of stools during the study period (24-72 hours). • Normally, 95% of dietary fat is absorbed and fecal fat excretion is≤ 5 grams/day on a 100 gram-daily fat intake. • The test is not specific as to etiology.
Disturbances in the Enterohepatic Circulation of Bile Salts • Liver Disease; • Bile ducts; • Small bowel: • Malabsorption • Deconjugation • Binding or precipitation
BILE SALT MALABSORPTION:CAUSES • Ileitis (Crohn’s disease); • Surgical resection of ileum; • Idiopathic
BILE SALT MALABSORPTION: CLINICAL FEATURES • Diarrhea; • Bile salts; • Hydroxy Fatty acids • Steatorrhea; • Cholesterol gallstones; • Enteric hyperoxaluria Oxalate nephrolithiasis
Bile-Salt-Induced Diarrhea • Malabsorption of bile acids results in an increased concentration of bile salts in the colon. • At concentrations >1.5 mmol/L, DIHYDROXY bile salts inhibit electrolyte absorption and stimulate secretion by the colonic mucosa.
FATTY ACID-INDUCED DIARRHEA IN BILE ACID MALABSORPTION In the absence of micelles, unabsorbed free fatty acids reach the colon.
FORMATION OF HYDROXY FATTY ACIDS FROM UNSATURATED FATTY ACIDS + H2O HYDROXY STEARIC ACID OLEIC ACID Ricinoleic acid
Ricinoleic Acid, a laxative acting by increasing intestinal Secretion of water
Treatment of Diarrhea Caused by Bile Acid Malabsorption • Bile salt binding agents- cholestyramine.
Cholesterol Gallstone Formation in Bile Salt Malabsorption • Cholesterol solubility in bile (aqueous solution) depends on the concentration of bile salts. • Bile salt depletion reduces the solubility of cholesterol in bile, which precipitates out and forms gallstones in the gallbladder.
Mechanism of urinary oxalate stones formation in bile acid deficiency • Oxalate in food is usually precipitated out as Calcium oxalate in the lumen and is lost in the stool. • When lipolysis is normal and bile salts concentration is <critical micellar concentration, unabsorbed long-chain fatty acid compete with oxalate for calcium; • Consequently, a large amount of oxalate is lost to the colon, where it is passively absorbed and ultimately excreted in the kidneys.
Disturbances in the Enterohepatic Circulation of Bile Salts • Liver Disease; • Bile ducts; • Small bowel: • Malabsorption • Deconjugation • Binding or precipitation
Bile Salt Deconjugation • Bile salts are secreted from the liver as conjugates with either glycine or taurine. • The conjugation increases the acidity of the bile salt and makes it more hydrophilic1. • The conjugation decreases passive diffusion of the bile salts in the jejunum and maintains a high intraluminal concentration. 1. pKa of unconjugated bile acid≈5; of glycine conjugates ≈ 3.9; of taurine conjugates ≈2.0.
Deconjugation of bile salts may occur when bacteria colonize the proximal small bowel. • Normally, such colonization is prevented by 2 factors: • GASTRIC ACID; • MOTILITY OF THE SMALL BOWEL;
Bacterial counts and Luminal pH in the Human Alimentary Tract CountpH • Duodenum : 102-1003/ml 5.5-6.0 • Jejunum: 102-1003/ml 6.0-6.5 • Ileum: 108/ml 6.5-7.0 • Cecum 1010-1011/ml
Small Bowel Bacterial Overgrowth (SIBO) • Achlorhydria or hypochlorhydria: (PPI treatment; atrophic gastritis; postoperative stomach). • STASIS: • Motility disorder: diabetic autonomic neuropathy, scleroderma, chronic intestinal pseudo- obstruction). • Anatomical changes: Strictures, small bowel diverticula, fistula, blind loop.